Are Genetics Responsible for Ankylosing Spondylitis?
Researchers haven’t singled out an exact cause of ankylosing spondylitis, but they believe genetics and environmental factors may be to blame.
In particular, researchers have found people with the HLA-B27 gene are at a considerably higher risk for developing ankylosing spondylitis. But having this gene doesn’t always mean you will get AS. The National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) reports that although almost eight percent of Americans have this gene, less than five percent go on to develop AS.
In 2007, scientists tracked down two more genes – ERAP1 and IL23R – that, along with HLA-B27, may increase a person’s susceptibility to AS. Researchers believe this important discovery will help them better understand how to treat AS, and may even lead to a blood test that can predict AS risk and help with early detection.
Although experts have not pinpointed exactly what causes AS, ongoing research continues to shed light on the condition, and offers encouraging insight into new medications and treatment options.
Who Is At Risk for Developing Ankylosing Spondylitis?
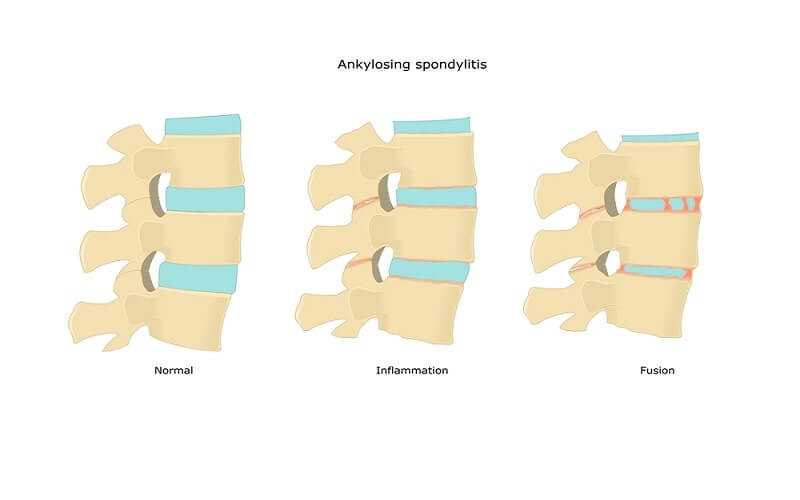
A type of spinal arthritis, this life-long condition causes inflammation and swelling mainly in your vertebrae and hip joints – often resulting in severe pain and stiffness in your back and hips, and sometimes in the neck, shoulders, ribs, hands and feet. In some cases, but not all, this chronic inflammation can cause some of the vertebrae in your spine to fuse together in an effort to heal, resulting in a bent forward posture, limited movement and possibly even restricted lung capacity.
Unlike other forms of arthritis, AS typically occurs in younger people between the ages of 17 to 45. It’s estimated to affect as many as 2.4 million people in the U.S. According to the NIAMS, roughly 80 percent develop AS before age 30, while only 5 percent have symptoms after age 45. Some claim it affects twice as many men as women.
Risk factors that increase a person’s likelihood of developing the condition include:
• Having the HLA-B27 gene
• A family history of AS
• Frequent gastrointestinal infections
Some experts believe that infections or even normal bacteria that live in the intestines may trigger AS in people who are genetically vulnerable. AS begins when defenses are destroyed in the intestines and bacteria passes directly into the bloodstream where the hip joints connect to the spine.
Because genetics seem to play a major role in developing AS, this condition may not be preventable. But understanding your personal risk factors can help you get an early diagnosis and proper treatment – possibly keeping pain at bay and delaying or even preventing complications in the future.