Back Surgery Options

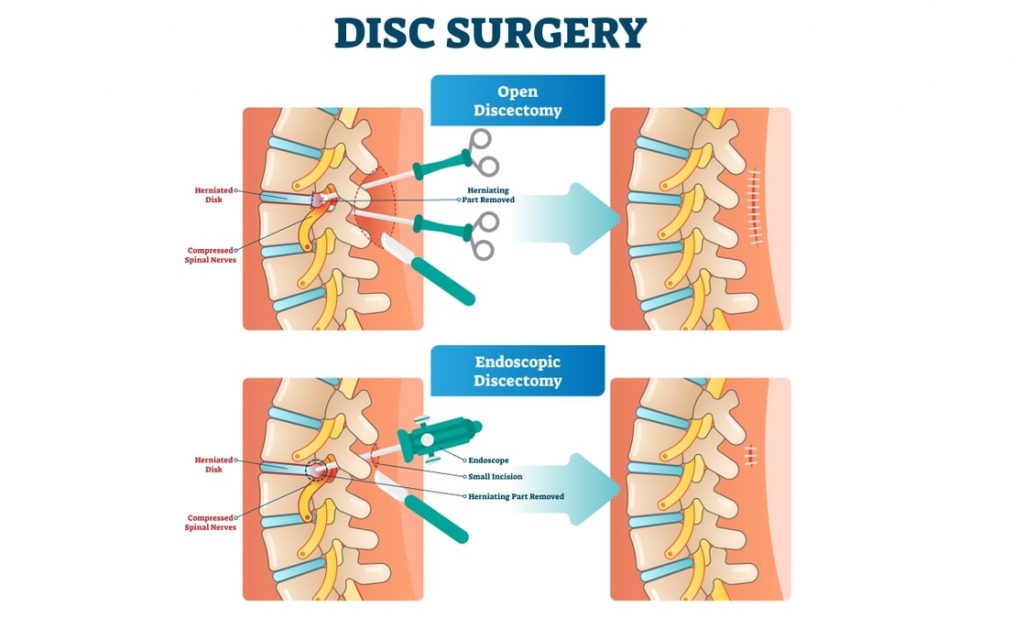
The majority of lumbar disc herniations (around 80%) respond to non-surgical intervention and do not require surgery. However, the most commonly performed spinal surgery in the US is the lumbar discectomy which can help reduce symptoms such as sciatica. Nearly half a million lower back surgeries are conducted each year in the US and innovations in the area of spinal surgery are developed and incorporated into treatments at a swift pace. Traditionally, large incisions were used to gain access to the musculature of the back which would then be pinned back to expose the lamina covering the spine. Open back surgery required the removal of the lamina to grant visual access for the surgeon to the troublesome discs, or osteophytes, causing nerve compression. A significant degree of trauma occurs in this kind of surgery which means that complications are more likely and recovery takes longer.
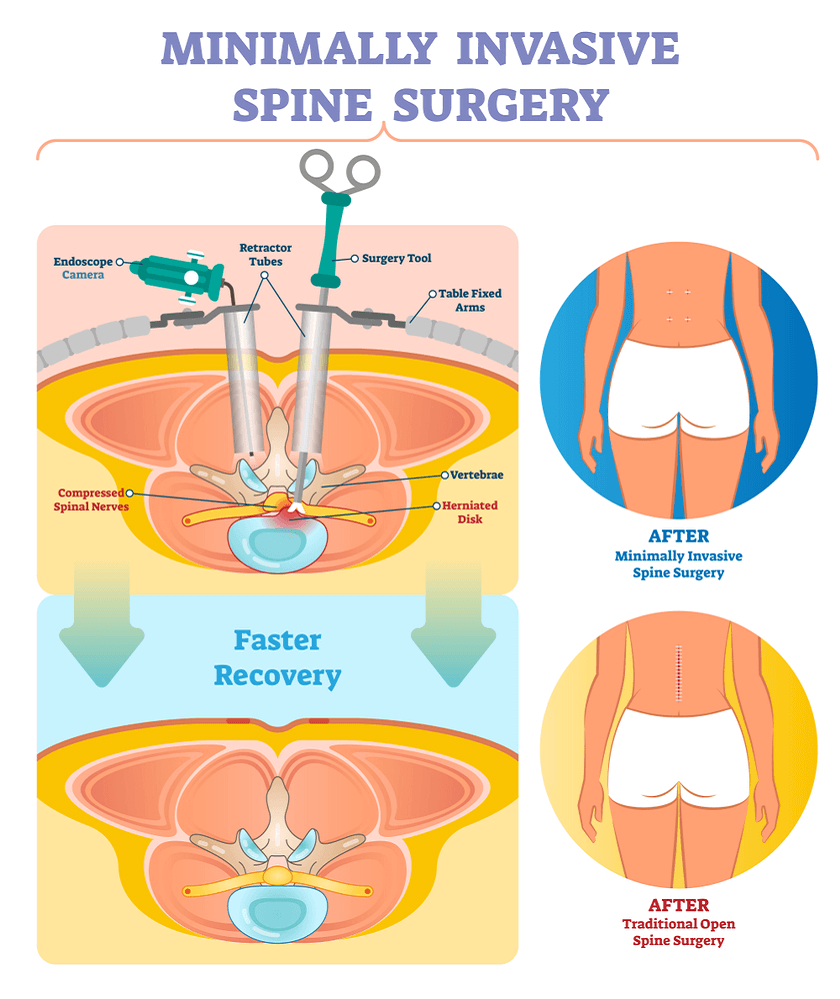
Minimally invasive back surgery procedures have, therefore, been developed to reduce the impact on spinal tissues and structures. The use of endoscopes and microscopes can give the surgeon visual access to the spine without the need for a large incision or the retraction of tissues. By passing a series of gradually expanding tubes into the incision and then feeding the endoscope through these tubes along with tiny surgical instruments, the procedure can be conducted with little trauma inflicted on surrounding structures in the spine. Laser spine techniques have also revolutionized back surgery allowing patients to undergo short procedures with little tissue damage or risk of complication and a much faster recovery rate than traditional surgeries.

Traditional Open Back Surgery
Back surgery traditionally involves a large incision to open up the spine and the removal of the lamina to expose the discs underneath. This type of traditional open back surgery requires the retraction and clamping of connective tissue, blood vessels, and nerves in the operative area in order to grant the surgeon visual access to the lamina and discs. Muscles in the back may also be cut during this type of open surgery or clamped in such a fashion that they suffered permanent damage as a results. This amount of trauma can cause bruising, bleeding, more extensive scarring, both internally and externally, and longer recovery times than more modern approaches to back surgery. Complications are also more likely in this type of surgery due to the invasiveness and the length of the operation.
In many cases the preferred option for a patient is a more minimally invasive back surgery. However, in some cases the traditional open method is necessary as multiple levels of the spine may require attention or fusion may need to occur. Traditional fusion techniques require considerable access to the spine and destroy a large amount of tissue in the process of fitting stabilizing instrumentation. Advances in microsurgery have not occurred at the same rate for patients requiring spinal fusion despite attempts to use smaller incisions and bone fragments passed through a cannula to achieve fusion. Failure rates have been high for minimal access spinal fusion and the open method is still preferred by the majority of spinal surgeons. Research continues into devices and methods to improve minimal access spinal fusion outcome and some surgeons have had success with the procedure.
Microsurgery
In contrast to open back surgery, microsurgery allows a surgeon visual access to the spine and its structures through an incision approximately 1.5inches across. The back muscles may still be stretched slightly on the side of the herniation or osteophyte growth. The surgeon will pass a small microscope through the incision in the back to allow them to see the site of the nerve compression. After removal of the herniated portion of disc the surgeon will retract the instrumentation and suture the incision closed. Muscle, ligament, and bone disruption are minimized in this type of surgery though, which improves patient outcome, speeds up recovery, and reduces complications. Patients can undergo the procedure under local anaesthetic, which reduces the risks of thrombophlebitis, and they can be up and mobile within a matter of hours of the operation before returning home either that day or the next.

Minimally Invasive Spinal Surgery
The incision for minimally invasive spinal surgery is even smaller than that used in microsurgery at approximately 1 inch across. The tubular retractor that is used to provide access to the spinal column measures around ¾ of an inch across and pushes between the muscles in the back rather than requiring them to be stripped away and held back forcibly. The METRx® system is commonly used by surgeons and can achieve high rates of surgical success. A fiberoptic light and tiny camera are inserted through this created tunnel to give the surgeon excellent visual access to the problematic area of the spine. Tiny instruments such as mini-forceps, curettes, trephines, rasps, burrs, cutters, and probes are then inserted as required to remove the herniated fragment of disc, problematic osteophyte growth, or other material. Nerve root decompression can then occur as the material impinging upon it is extracted using cutting and suction through a discectome (hollow suction tube).
There are potential complications however, with the possibility that the surgeon will have to conduct an open procedure anyway, the risk of neurological damage, and soft tissue trauma. Due to the smaller operating area and the nature of the instrumentation used there is also the added risk of the instrumentation breaking which would extend surgery time or necessitate a transition to an open procedure. Minimally invasive spinal surgery can be conducted as an outpatient in contrast to the lengthy stay in hospital usually required with traditional open back surgery. Success rates are usually around 80-90% for treating sciatica with minimally invasive spinal surgery.

Laser Spinal Surgery
Laser spinal surgery has become a popular option for those looking to relieve back pain due to disc herniation. The technique has been heavily marketed but has, as yet, little in the way of clinical trial data to show effectiveness or safety. Many orthopaedic hospitals do not use the procedure despite a large number of laser spinal surgery having been carried out over the past few decades, and few reports of complication. Laser surgery has the benefit of requiring a smaller incision than the traditional open back surgery and can significantly reduce the length of the operation and the recovery period for patients. As the procedure is carried out often under local anaesthesia, patients may feel relief from their symptoms instantly and can be mobile within a matter of minutes after the operation. Recovery time is usually around two weeks with patients able to return to work considerably earlier than if undergoing an open back operation.
Disadvantages of Laser Spine Surgery
The drawback of laser spinal surgery is that the lasers cannot cut through bone so are only useful if the spinal compression, or stenosis, is being caused by a bulging or herniated disc or disc fragment. Osteophyte growth presents a challenge for laser surgery and a more traditional method, or tools, would be required to remove this source of nerve compression. The technique of laser spinal surgery is similar to other minimal access procedures as it uses a small incision to feed a laser and camera into the area of the disc herniation. The laser is then used to vaporise the problematic disc material thereby, hopefully, relieving the compression on the nerve. The material itself is not removed during laser surgery but the overall pressure of the disc is reduced. This can result in the need for additional surgery at a later date.