Spinal Stenosis Surgery
The two procedures carried out for spinal stenosis are ‘decompression’, the removal of any bone, disc or ligament compressing nervous structures, and ‘decompression with fusion’, in which vertebrae are fused together (joined with bone) in addition to the decompression. The decision as to which operation to perform is based on an evaluation of the ‘stability’ of the segment of spine being operated upon.
In the absence of instability, such as spondylolisthesis, there appears to be no benefit to performing a fusion. Studies comparing decompression/fusion surgery with decompression alone in patients without instability show that outcomes were identical, with 80% getting good results regardless of whether or not fusion had been performed.
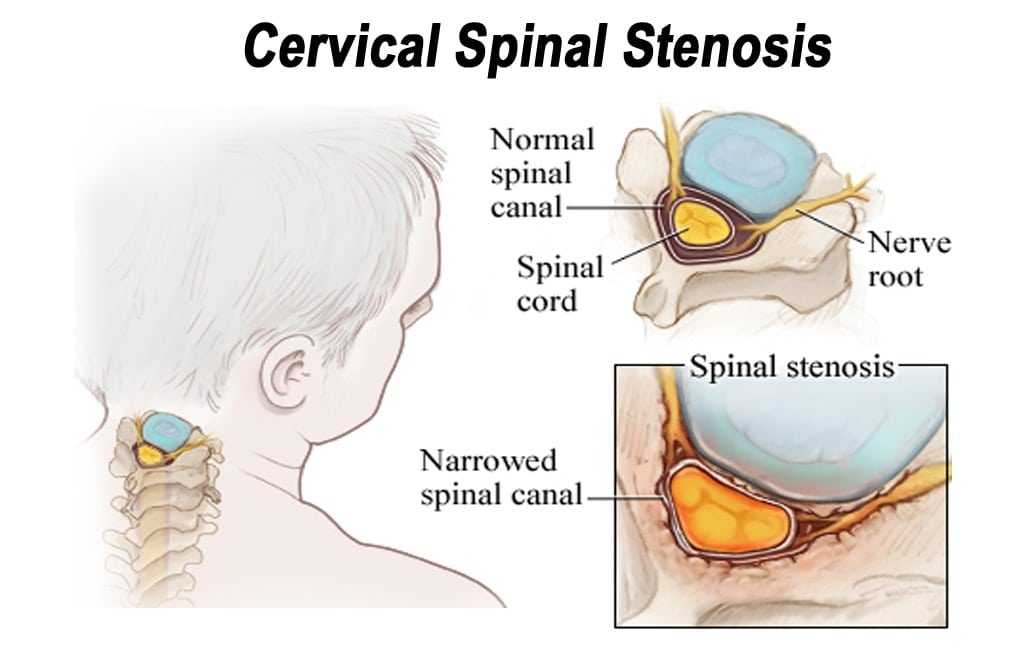
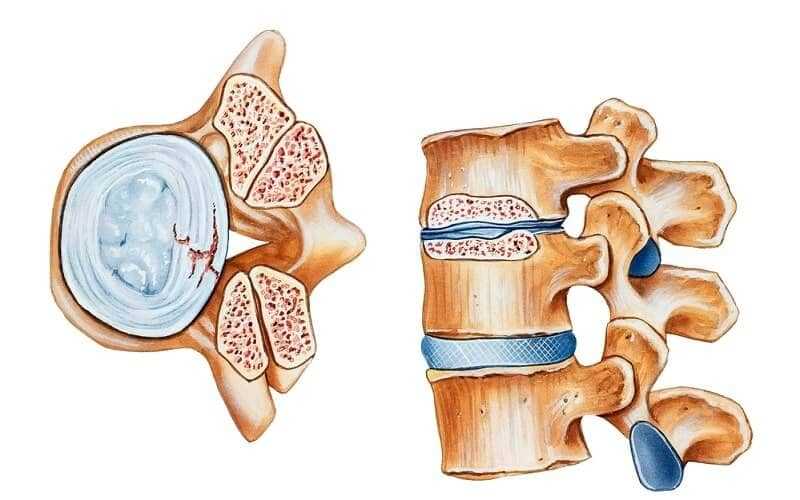
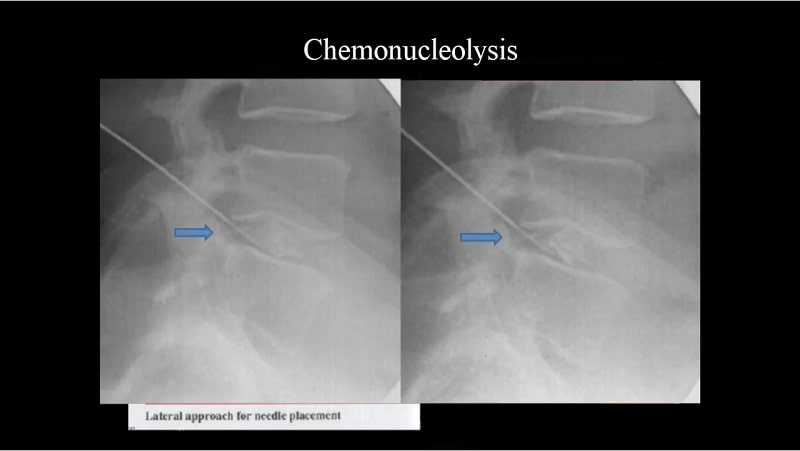
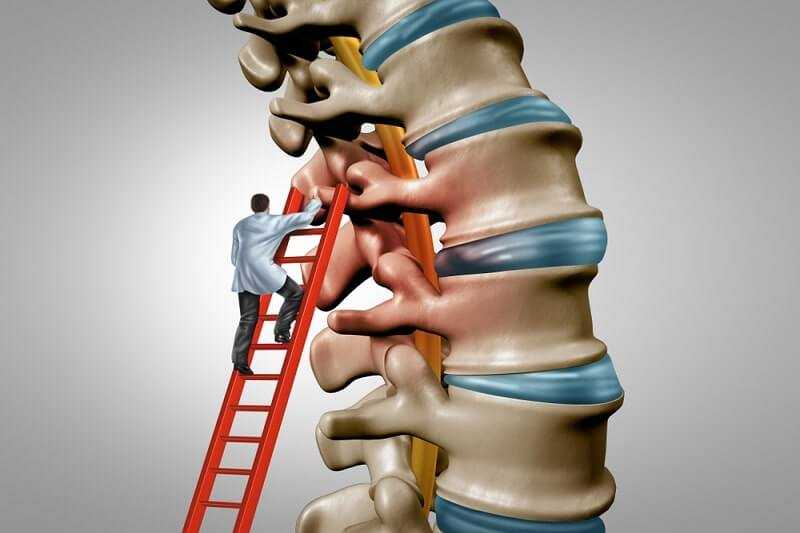
Decompression
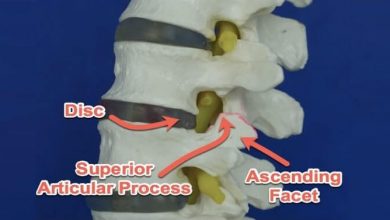
This surgical procedure involves the removal of bone, disc material, or ligament that may be compressing nervous structures. Pre-operative CT or MRI will demonstrate those areas of significant narrowing. Surgery addresses the areas that are clinically relevant; there needs to be a good match between the imaging studies and the patient’s clinical presentation. Original surgical technique involved removal of a large amount of bone, including the spinous processes as well as the laminae. We now know that this may in fact be too extensive and may result in instability and chronic low back pain. Recent studies have demonstrated that more conservative bone removal still results in excellent outcome without the potential problems of more expansive resection. The average length of stay in hospital is also lower with this type of procedure.
Procedure
Typically a mid-line posterior incision is made measuring 3 to 10 centimeters in length, depending on the number of vertebral levels involved. In most cases, the muscle is stripped from just one side of the spine and small port-holes are made in the bone, removing only those elements that are compressing the nerves. This reduces the amount of postoperative pain, improves recovery time, and minimizes blood loss.
Results
Overall, decompression for degenerative spinal stenosis results in over 80% of individuals reporting significant postoperative reduction in walking-related leg pain. Again, one must have reasonable expectations. Walking tolerance may not be completely unlimited and other medical conditions may play a part in this. Most report, however, that their quality of life has been significantly improved. A degree of ongoing low back pain may persist, especially if this was a major feature preoperatively. Generally, however, it is tolerable compared to the lower extremity symptoms experienced pre-operatively.
The post-operative course is typically one of early mobilization and most leave hospital within 1 to 3 days. Again, there are usually no medical restrictions to activity, and patients are strongly encouraged to regain normal physical strength and flexibility through an active program of exercise postoperatively.
Risks
With respect to surgical risk, there is always a risk of infection rated at 0.5% superficially and 1/500 for a deep wound. There is always a risk of injury to the nerve, but this risk is low. Some individuals do not experience any neural recovery despite an adequate decompression and these individuals may continue to have lower extremity symptoms. Although spinal stenosis does not typically paralyze an individual or put them in a wheel chair, the more profound the weakness and sensory loss in the extremities, the more difficult it is for full recovery to occur.