How Do You Treat Sjogren’s?

Sjogren’s syndrome is a chronic illness, but there are many things you can do to deal with your symptoms in order to feel better, prevent complications, and improve your quality of life. We believe that learning as much as possible about your illness will help you and your doctor decide on the best course of treatment, improve the chances that you will follow that treatment, and ultimately improve the outcome. By reading this article and pursuing additional resources for support and information, you are already on the road to a sound treatment plan.
The first step is to find medical and health care professionals who are knowledgeable about Sjogren’s syndrome, or willing to learn, and with whom you are comfortable. Second, you need to know about medications available by prescription and about over-the-counter products that might help. If you have other disorders in addition to Sjogren’s, you will want to consider the impact on each disorder and on your Sjogren’s. Finally, medical professionals and other Sjogren’s patients can be important sources for helpful hints. Just remember: no two patients are alike, and always check with your doctor to make sure products are safe for you!
Finding the Right Doctor
Regardless of who makes the diagnosis of Sjogren’s syndrome, it is a good idea to have a medical doctor coordinate your care. Usually this is a rheumatologist. Some patients rely on a clinical immunologist, family physician, or general practitioner. Your rheumatologist or other primary physician might want to see you only once or twice a year if you have had no problems for a sufficient stretch of time, or he or she might want to schedule you for visits every one to four months, depending on your symptoms and medications.

Because Sjogren’s syndrome can affect any part of your body and be exacerbated by other common illnesses, patients often ask if they should use their rheumatologist for everything or if they should see an internist too. This question should be discussed with your doctor. Some rheumatologists feel comfortable handling all aspects of your health and taking the time to do so; they will refer you to a specialist when needed. Others prefer that you call an internist for problems not directly related to Sjogren’s.
You should see a dentist and ophthalmologist regularly, whether you suffer severe symptoms or not. Prevention and recognition of problems before they become severe are key. A good rule of thumb is to see your dentist three times a year and ophthalmologist twice a year, unless you are on medications that need more frequent monitoring or you are having problems that require more frequent attention.

You will see other specialists depending on your symptoms and which organs and body systems are involved.
Unfortunately, the number of rheumatologists is declining (Hahn 2000). This is bad news for those with Sjogren’s syndrome and related diseases. In addition, managed care programs might not have a rheumatologist on staff at all, and it can be difficult to get necessary referrals to see specialists needed to treat Sjogren’s syndrome.
While the Sjogren’s Syndrome Foundation does not recommend specific physicians, the foundation can provide you with names of medical professionals for your area that other patients have found helpful. Foundation volunteer contacts are available for you to call in your area, and they might help you find a medical center or physician close by.
If you cannot find someone locally with whom you feel comfortable, or if you have developed complications and believe you need additional opinions or help, you might want to look for a specialist at a university or other major medical center that sees many Sjogren’s patients. A list of treatment centers can be found on the Sjogren’s Syndrome Foundation Web site.
Medications and Products
No prescription medications existed specifically for Sjogren’s syndrome until recently. The first drugs ever to target Sjogren’s began to emerge over the last few years along with breakthrough medications for related disorders, such as rheumatoid arthritis and multiple sclerosis.
Before we take a look at specific medications and products, we want to offer some words of caution and advice. First, citing any group of medications or common brand names does not imply endorsement on the publisher’s or our part. Second, we advise that you always check with your doctor about use of any medication or product.
Those with Sjogren’s syndrome and other autoimmune diseases can be extrasensitive to medications and tend to have more side effects and drug reactions than the normal population. According to European studies, 18 percent of Sjogren’s patients were allergic to penicillin and 15 percent to sulfur compounds (Jonsson, Haga, and Gordon 2001).
Always tell your doctor about all medications you are taking; any vitamins, herbs, or natural remedies you are using (these might interfere with or enhance effects of other medications); and any side effects you experience.
Finally, while we list some of the most commonly reported side effects, these lists are not meant to be comprehensive.
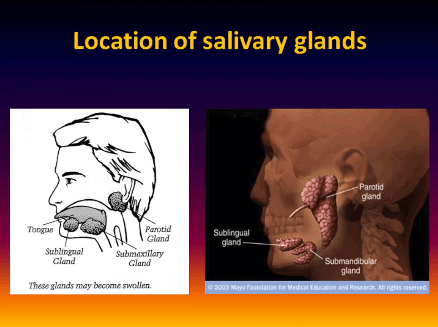
Help for Dry Mouth
Two prescription drugs to treat dry mouth have recently been approved by the Food and Drug Administration. These are Salagen (pilocarpine hydrocholoride) and Evoxac (cevimeline). Both increase saliva production; if one does not work for you or you experience uncomfortable or intolerable side effects with one, try the other. The most common side effect of both drugs is increased sweating, and some patients find that one or both of these drugs increase tear production as well.

Use of a prescription fluoride gel will help protect your teeth from cavities. Your dentist can make custom-fitted trays for your teeth, and you should apply a thin ribbon of fluoride in each tray and place on your teeth for approximately two to five minutes every night before going to bed. Do not rinse your mouth after applying fluoride. Brush-on fluorides are also available. Watch out for fluoride mouth rinses that contain alcohol, which is drying and irritating to the oral tissues.
To fight oral Candida, or yeast infections, drugs such as Nystatin are available. A catch-22 exists with this condition, because most prescription lozenges for oral use contain sugar, and sugar increases yeast growth. Formulas made without sugar are available, but their terrible taste makes them intolerable for many potential users.

There are also many nonprescription products for dry mouth, including artificial salivas and mouth coats. Contact the Sjogren’s Syndrome Foundation for its up-to-date product list.
Other Things You Can Do
Humidify your bedroom or house. Carry water. Chew sugar-free gum. Beware of sugarless gum; this label means less sugar, not zero sugar. Use lip coats to protect lips and the corners of the mouth from chapping.

Dental Implants
If you are diagnosed and treated for dry mouth early in the course of your disease, you should not lose your teeth. However, diagnosis and treatment can come too late, and losing your teeth can be an unfortunate consequence. Dentures have long been the only solution, and they often don’t work well in a dry mouth. Now, oral surgeons are turning to dental implants with greater frequency and success, and while they are expensive and labor-intensive for both doctor and patient, the procedure offers an important alternative and holds promise for improvement in the future.
Treatment of Dry Eyes
Lacriserts, available by prescription and made by Merck, have actually been on the market for a long time. Lacriserts are small rice-grain-size pellets that are placed under the lower lid, between the lid and the eyeball, and release moisture for hours. People with Sjogren’s either love them or hate them. Periodic shortages have plagued devoted users.
Several prescriptions are currently under investigation as of this writing. Cyclosporin A is undergoing final testing, and scientists are researching other potential treatments, such as topical androgens and tear-volume-enhancing compounds (Meisler 2001).
Over-the-Counter Products
Moisture drops are the first line of defense for dry eyes. If you use them more than four times a day, you need to be sure they are preservative-free drops. Preservatives found in many eye drops can cause a toxic reaction with too frequent use.
Try drops from different manufacturers until you find one you like. Put in drops before you’re conscious your eyes are dry. Your eyes will feel better and avoid the potential complications of dryness when they are kept moist.
If drops don’t increase your comfort level enough, ointments are available. Apply a rice-grain-size ribbon to the inside of the lower lid. Ointment can cause blurriness of vision for a while after application, so some people use it just at night. Moisture drops can be used in combination with the ointment. Again, preservative-free is best for ointments. If you cannot tolerate the lanolin found in some preservative-free ointments try switching to another brand. Topical gel-like products are also available. They are more viscous than drops but less so than ointments. They don’t tend to blur the vision as much.
Special Procedures
Tear loss is diminished when the ducts through which tears escape are closed. Closing these ducts is called punctal occlusion. Your ophthalmologist can close them in one of two ways: by inserting removable punctal plugs made of silicone (or sometimes, collagen) or by cauterization or laser, a more permanent solution. In the former, plugs have been known to fall out, in which case new ones must be reinserted. In the latter, ducts can infrequently and spontaneously reopen on their own. Your ophthalmologist will probably treat the lower ducts initially to see if their closure improves your symptoms or decreases your need for artificial tears. The upper ducts can be done as well if you need additional retention of tears.
Other Things You Can Do
A tolerably hot, wet washcloth applied over your eyes while they are closed can help ease pain. Eyelid cleansers that clear mucus and debris away can help when blepharitis, a condition that can accompany dry eyes, occurs. Special glasses with side shields (moisture chamber glasses) or goggles can be made to slow evaporation and protect your eyes from the drying effect of wind. The Sjogren’s Syndrome Foundation has a list with more information on how to obtain products.
General Medications
Medications that reduce inflammation are frequently used in Sjogren’s syndrome and other inflammatory conditions. The Arthritis Foundation publishes a drug guide for arthritis-related conditions every year. Check it out for the most up-to-date information. Those most frequently used for Sjogren’s syndrome follow.
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
NSAIDs (pronounced IN-sayds) reduce inflammation and ease pain. The best known NSAID and often the first line of defense for arthritis-related diseases is aspirin. Aspirin is a natural antiinflammatory, and it can help keep inflammation and pain under control.

Aspirin is a blood thinner that acts by stopping platelets from sticking together, so if you’re prone to blood clots with your Sjogren’s syndrome, your doctor might have another reason to put you on aspirin. However, if you’re already on another blood-thinning drug, your doctor will probably put you on an antiinflammatory medication other than aspirin. Some people have stomach upset with aspirin. If you are subject to stomach ulcers or bleeding, you probably should not take aspirin. Any NSAID can cause stomach upset, including stomach and gastrointestinal bleeding, and should always be taken with food or milk (unless you are taking an enteric-coated pill).
If you cannot tolerate aspirin, your doctor might suggest trying one of the many nonaspirin NSAID drugs. Examples of common brand names include Naprosyn, Aleve, Motrin, Tolectin, Relafen, Feldene, and Ansaid. Some are available by prescription only.

NSAIDs work by inhibiting the enzymes necessary to produce prostaglandins, which can cause inflammation and pain. Overdoses can be toxic to the liver and long-term use can affect the kidneys. Consult your doctor if you want to increase your regular dose, such as taking additional aspirin for a headache, or if you want to use more than one kind of NSAID.
Don’t confuse acetaminophen with aspirin or NSAIDs, such as ibuprofen. Acetaminophen is a pain reliever and does not greatly reduce inflammation.
Cox-2 Inhibitors
A new category of drugs combats inflammation and is easier on the stomach than either aspirin or other NSAIDs. Examples include Celebrex, Vioxx, and Bextra. Cox-2 inhibitors block the Cox-2 enzyme, impeding production of prostaglandins which cause inflammation. The new Cox-2 inhibitors do not act in the stomach but rather in areas responsible for inflammation.

Corticosteroids (Steroids)
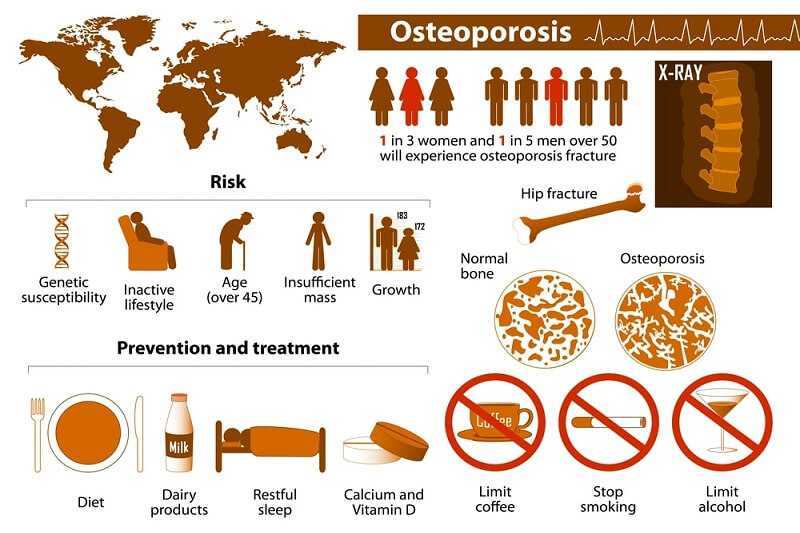
Corticosteroids have been around for a long time. They are powerful drugs, and if a person is experiencing debilitating symptoms or dangerous complications, these drugs can often help resolve them. Prednisone is the most widely prescribed steroid. If you are having a major flare-up, sometimes a short-term dose of prednisone is needed. However, this class of medications comes with potential major side effects associated with long-term use and frequency of use. Corticosteroids can reduce resistance to infection, cause bone loss and osteoporosis, lead to the development of cataracts, cause thinning of the skin, and result in increased appetite, and weight gain, and water retention (the so-called “moon face” is a common side effect). They can also lead to the onset of diabetes.
Disease-Modifying AntiRheumatic Drugs
The drugs we’ve mentioned so far either suppress the immune system or reduce inflammation or both. Disease-modifying antirheumatic drugs are anti-inflammatory drugs that go a step further by actually altering the course of a disease.
Antimalarial Drugs
Antimalarial drugs were developed to flght malaria, but clinicians discovered that these drugs help in some autoimmune diseases, including Sjogren’s syndrome.
The most common antimalarial drug prescribed for Sjogren’s syndrome goes by the brand name of Plaquenil (chemical name: hydroxychloroquine). Many people with Sjogren’s feel much better on Plaquenil and often experience improvement in fatigue, joint and muscle pain, and many other systemic symptoms. If you are prone to blood clots and have antiphospholipid syndrome, antimalarials can help.

If you are on hydroxychloroquine, you must see an ophthalmologist every six to twelve months. Though extremely rare, high doses of antimalarial drugs have been known to cause retinal damage. The chemical makeup of Plaquenil and low dosage prescribed for autoimmune disease reduce this risk. Check with your doctor about other potential side effects and monitoring requirements.
Methotrexate
Methotrexate reduces inflammation. It was developed for certain cancer patients and later found to be helpful for rheumatoid arthritis. Approved for use in rheumatoid arthritis by the Food and Drug Administration in 1988, the drug has been successfully used by many rheumatoid arthritis patients and those with related, overlapping disorders.

This drug is generally reserved for progressive and active, severe disease. Side effects can include reduced ability to fight infection, reduced fertility while on the medication, gastrointestinal symptoms, mouth sores, and shortage of folic acid. Some reports suggest that use of methotrexate can increase the risk of malignant non-Hodgkin’s lymphoma. Consult your doctor and your pharmacist for a full list of potential side effects.
Cytoxan or Cyclophosphamide
This powerful immunosuppressant can have a lifesaving impact on severe disease. As with other powerful medications, however, benefits need to be weighed against potential risks, since this medication can reduce your ability to fight off infection.
What about Biologic Response Modifiers?
You might have heard about some of these drugs, commonly used for related autoimmune disorders. This class of drugs is relatively new on the market, and testing and research on most of these drugs have been directed towards rheumatoid arthritis. This group includes etanercept (Enbrel), infliximab (Remicade), and the newest—anakinra (Kineret). These drugs reduce inflammation caused by cytokines by blocking TNF-alpha, or tumor necrosis factor- alpha. TNF-alpha is involved in Sjogren’s, and the Sjogren’s Syndrome Clinic at the National Institutes of Health is investigating the effect of etanercept on Sjogren’s. One recent study examined infliximab use in primary Sjogren’s syndrome patients and found significant improvement in clinical features, including dry eyes and dry mouth (Steinfeld et al. 2001). Another recent study showed potential negative effects on the nervous system and exacerbation of multiple sclerosis when anti-TNF-alpha therapy was used (Mohan et al. 2001).
Other Specific Symptoms
Because Sjogren’s syndrome can affect any body organ or system, patients will face an array of symptoms and potential medications to ease those symptoms. These include:
Reflux. Many prescription and over-the-counter products are available for gastrointestinal symptoms such as reflux. Acid blockers include recognizable brand names such as Tagamet, Zantac, and Pepcid. Over-the-counter varieties can help reflux but are usually insufficient to counteract gastrointestinal effects of NSAlDs. Another category of medication that reduces acid production is the proton-pump inhibitor such as Nexium, formerly named Prilosec, and the commonly prescribed drug Prevacid. Before turning to medication, try elevating the head of your bed by placing blocks of wood under the legs at the head. This alone just might do the trick!

Nerve pain. If you suffer from nerve pain or severe numbness, treating your Sjogren’s with one of the systemic medications might help. Prednisone reduces nerve inflammation and might give relief. Gabapentin (Neurontin) is sometimes used by Sjogren’s patients for nerve pain, although it was originally designed to prevent seizures.

Antiphospholipid antibody syndrome. If you have this syndrome, you need a blood thinner, or anticoagulant, to prevent blood clots. Your doctor might recommend that you take one baby aspirin a day, or you might need a prescription medication such as warfarin (the brand name you might be familiar with is Coumadin(Warfarin)) or heparin.

Autoimmune hearing loss. Patients with autoimmune hearing loss have responded well to corticosteroids and cyclophosphamide. Controlling the autoimmune disease process with anti-inflammatory drugs can be helpful. Diazepam (Brand names Valium and Diastat) has been used in some cases to calm the inner ear in Meniere’s disease.

Osteoporosis. If you have been on long-term or high doses of prednisone (or have a family history of osteoporosis), you will want to talk to your doctor about the many drugs available to help prevent osteoporosis. There are new drugs now that not only prevent bone loss but actually build bone. These include Fosamax and Actonel, which are now available in once weekly doses. You may also need to take calcium and vitamin D supplements.
Dryness everywhere! Nasal sprays are available for dry nasal passages. In addition, some people use a nasal irrigator, a device that attaches by a hose to a unit such as the WaterPik, and forces water (or saline or anti-mucus solution) through the nasal passages. Keep your head down over a sink, breathing through your mouth. Place the irrigator in one nostril, let the water flow through one nostril and out the other, and then switch to the other nostril and do the same thing.
Vitamin E capsules can be broken open (the cheapest way to obtain vitamin E oil) and the oil applied to the external area around the vagina. During peri- and postmenopause, your doctor might recommend vaginal suppositories (such as Vagifem), especially if you do not take hormone replacement therapy. Many lubricants are on the market to help dry skin. Again, refer to the product lists distributed by the Sjogren’s Syndrome Foundation.
Infections. Because the immune system is not functioning normally in autoimmune diseases, many of us find we are more vulnerable to infections and take longer to fight them off. Prompt recognition and treatment of an infection is important in the Sjogren’s syndrome patient to succeed in more quickly combating the infection and preventing complications. For example, eye infections need prompt attention; oral yeast infections can become recurrent and hard to control if not treated immediately; and respiratory infections can lead to bronchitis and pneumonia.
Fatigue. We wish we could tell you there is a magic bullet that will zap your fatigue with Sjogren’s syndrome, but the best advice we can give is to tell you to work with your physician to keep your disease activity under control as much as possible. Many medications that control Sjogren’s symptoms can help increase your energy levels. The antimalarials and Cox-2 inhibitors often help reduce fatigue and are preferable for long-term use over corticosteroids. In addition to medication, your fatigue can be handled through lifestyle management, including exercise and pacing of activities, as we will discuss later.
Pain. Treatment of pain depends on the cause. If the cause is your Sjogren’s, then treating the underlying disease will often help, just as it will help with fatigue. If you are experiencing muscle and joint pain, then the same anti-inflammatories that help the disease will be your first line of defense. If your mouth pain is caused by a yeast infection, you need to treat that infection. For nerve pain, your options include trying medications that treat your Sjogren’s in general or specific drugs targeted to the nerves. When standard therapies are not working, some people turn to natural remedies to help them deal with fatigue and pain—a topic we turn to next.
Natural Remedies
Many people will tell you they heard about a remedy that could be a sure or potential cure for your Sjogren’s syndrome. We are certainly open to the possibility that some of those remedies might prove beneficial in the long run, but until they are: Beware! Just because something is natural, this does not make it safe or appropriate. Aspirin is “natural,” but it can have undesirable side effects as well as benefits. Other natural remedies can be quite powerful, and you should watch out for potential interactions with other medications you’re taking.
Science is all about investigating old and new ideas and learning by testing hypotheses. If you want to use a remedy that is not approved for use in Sjogren’s or is not widely embraced by the medical community, talk to your doctor about it. Some vitamins and supplements have been proven to be helpful in Sjogren’s. Vitamin C is a natural anti-inflammatory, but too much can cause stomach upset, diarrhea, and kidney problems. Vitamin B6 can help inflamed nerves, but again, too much can be detrimental.
Therapeutic massage is safe, and we’re learning more about its therapeutic effects. The power of positive touch can be healing. Acupuncture treatments have also helped some people with Sjogren’s syndrome and are gaining in popularity for many conditions. However, no clear evidence links acupuncture to benefits for Sjogren’s syndrome.
The National Center for Alternative and Complementary Medicine at the National Institutes of Health is a good source of information on natural remedies.
When You Have More Than One Disorder
Sometimes, treatment for one disorder can impact another. Once again, talking over all of your symptoms and treatments with your doctor is critical. For example, many medications effective for allergies or colds cause dryness. If you have Sjogren’s syndrome, it’s important to know this and to discuss potential alternatives with your doctor. Antidepressants can cause dryness as well.
Because manifestations of Sjogren’s syndrome can differ from person to person, a drug that works for someone else with Sjogren’s might not be right for you. We have mentioned that the new anti-TNF-alpha drugs might be beneficial for some Sjogren’s patients, but if you suffer from neurological difficulties, you and your physician will want to be aware of a potential negative impact on the nervous system. NSAIDs are helpful for many people with Sjogren’s but not necessarily for those with a propensity for gastrointestinal side effects.